2019-03-14
Infectious diseases are different from other diseases in that they are caused by microorganisms that spread from one individual to another, sometimes passing through other humans, animals, or an environmental reservoir. While infectious diseases spread wherever and whenever they are able to, several situations increase the risk that infections as well as antibiotic resistance spread. To understand why and how some people are more vulnerable, we need to understand how infections are transmitted.

Routes of transmission
Most transmission routes of infections can be classified into three major categories: fecal-oral, contact and aerosols.
The fecal-oral route
The fecal-oral route is essentially what it sounds like – bacteria from feces are transported from the feces of one individual to the mouth of another. In the simplest form, a person goes to the toilet, does not wash hands properly and prepares a delicious meal for the family or a guest. Bacteria caught in the hands during the toilet visit are transmitted to the food and are eaten by the others, resulting in disease. Examples of diseases that can spread like this are food-borne and water-borne infections like typhoid fever and salmonellosis.
Contact transmission
Contact transmission occurs through physical contact either directly with an infected individual or indirectly via a contaminated surface. For example a health care worker that cares for one patient and then moves to another without washing hands or changing protective barriers, and thus transferring bacteria from one patient to another. Other examples of contact transmission are sexually transmitted infections and most wound infections.
Aerosols
Aerosols are a common route for transmission of respiratory tract infections. Typically, a patient with a cold or influenza would cough and sneeze, causing a cloud of small droplets carrying the pathogen, in this case a virus. The droplets can then be inhaled by a nearby individual that becomes infected. Bacterial diseases spreading through airborne droplets include meningitis, streptococcal infections and tuberculosis.
The One Health perspective
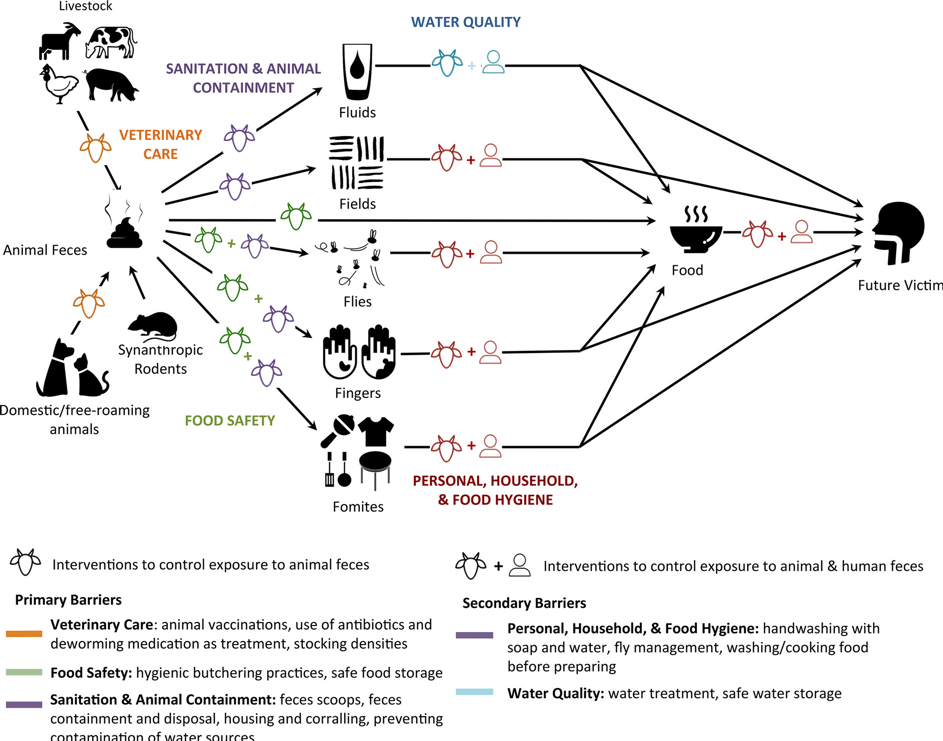
Infections are not only transmitted from human to human. Sometimes, humans transmit diseases to animals and animals transmit diseases to humans. In many cases, the link may be obscured as transmission happens via the environment or a carrier. As an example, animal feces may be spread on fields as manure without proper treatment that would kill disease-causing bacteria. The bacteria then contaminate the crop and end up in the food humans eat (a fecal-oral transmission). Similarly, both human and animal feces may contaminate water sources used for irrigation or drinking water, spreading diseases like typhoid or cholera. In other cases, a farm worker may transfer a disease-causing bacterium from animal to animal, effectively acting as a bridge between herds or even farms if hygiene and biosecurity are not maintained.
Vulnerable groups
Groups and populations that are especially vulnerable to infectious diseases include people living in poverty or being affected by armed conflict. A partial reason can be found in the nutritional status of the people affected as food supply is scarce, making them more susceptible to contract infections. But the nutritional status and following weakened immune system is not a sufficient explanation. Other important contributors are for example crowded living conditions in poor areas and refugee camps, and lack of functioning water and sanitation infrastructures. Both these factors increase transmission of infections through the routes describes above.
Preventing infections
In order to prevent transmission of infections, one measure stands out as the most effective for most infections and transmission pathways: water, sanitation and hygiene (WASH). The WASH concept includes access to safe and clean drinking water, adequate sanitation services (including waste treatment) and hygiene measures like handwashing both at home and in health-care and farming. These measures are even more critical to take among those most vulnerable and to reduce the spread of antibiotic resistance.
Further reading
New ReAct Report: When the Drugs Don’t Work – Antibiotic Resistance as a Global Development Problem.
ReAct Toolbox: Understand bacteria and infections.
ReAct Toolbox: Prevent infection.
ReAct Factsheet: Antibiotic resistance, water, sanitation and hygiene (WASH).
ReAct Factsheet: Antibiotic resistance and nutrition.
More news and opinion from 2019
- ReAct’s 2019 wrap up and 2020 expectations
- Blog post by UNDP and ReAct: Antimicrobial resistance: An emerging crisis
- Water, sanitation and hygiene services critical to curbing antibiotic quick fix
- Diagnostics: Antibiotic susceptibility
- ReAct highlights during World Antibiotic Awareness week 2019
- 2019 AMR photo competition prizes announced
- Launch of UNICEF’s institutional guidance on antimicrobial resistance
- Proposed ban on colistin for animal use announced in Indonesia
- School children led celebration of World Toilet Day and World Antibiotic Awareness Week
- 10 Innovate4AMR-winning teams enjoyed 3-day workshop in Geneva
- After 4 collaborative meeting days: Actions for the future in Latin America
- Four key points from joint comments to One Health Global Leaders Group on AMR
- Why are children more vulnerable to AMR?
- Dr Yoel Lubell, Health Economist, on Thailand, AMR, UCH and cultural factors driving AMR
- UHC and AMR: The Thai Experience
- Why do effective antibiotics matter for quality of care and patient safety?
- New ReAct policy brief: Antimicrobial resistance and universal health coverage – What’s the deal?
- Three key takeaways from the ReAct Africa conference
- Diagnostics: Species identification
- AMR-specific indicator proposed for monitoring Sustainable Development Goals
- Five focus areas at the 2nd Ministerial Conference on AMR hosted by the Netherlands
- Safety concerns of fecal microbiota transplants
- Upcoming ReAct Africa Conference: universal health coverage and antimicrobial resistance in focus
- Mother Earth conference in Argentina – the environment in focus
- Diagnostics: What are we talking about?
- Connecting global to local civil-society-agenda on AMR at CSO convening in Geneva
- ReAct colleagues featured in WHO Bulletin as leading profiles in the work on reacting to antibiotic resistance
- RAN stakeholder at WHO IPC consultation – for standards and guidelines in African Union member states
- WHA conversation on Antibiotic Resistance as a Global Development Problem co-organized by ReAct
- Insights from ReAct Asia Pacific project on antibiotic stewardship in secondary level hospitals in India
- Open letter to UN Member States from former IACG members Anthony So and Otto Cars
- ReAct UHC Intervention at UNGA Multi-stakeholder Hearing for High-level Meeting on UHC
- ReAct Latin America honors Earth Day
- Medicines Patent Pool’s view on the role of licenses for antibiotics – World Intellectual Property Day
- Second time for Innovate4AMR competition!
- World Health Day 2019: Universal Health Coverage
- Diagnostics: Constraints for successful implementation
- Antibiotic Shortages: magnitude, causes and possible solutions: A new WHO meeting report
- Erry Setyawan, FAO, on Indonesian NAP: We need to work together to make it possible to manage AMR
- ReAct’s new 5-year strategic plan receives funding from Sida
- How infections spread and how to stop them
- Generating data for policy and practice

