Listen to Maria Pränting explaining the mechanisms behind antibiotic resistance and spread of resistant bacteria.
Emergence of resistance
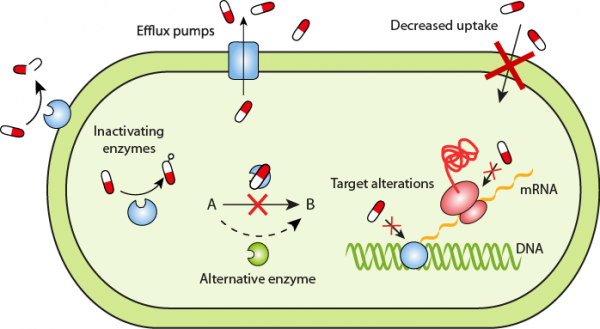
The picture below illustrates the mechanism though which bacteria can become resistant to antibiotics:
1. alteration of the target site for the antibiotic
2. production of enzymes that inactivate the antibiotic
3. alterations in the cell membrane resulting in decreased permeability and thus decreased uptake of the antibiotic
4. removal of the antibiotic using active transportation of the antibiotic out of the bacteria through so called efflux pumps
5. use of alternative pathways, which compensates for the action inhibited by the antibiotic
Spread of resistant bacteria
Resistant bacteria spread via many routes. Poor hygiene, poor sanitation and poor infection control are three interconnected key factors contributing to the spread of resistant bacteria in health care facilities as well as in the community. Bacteria know no boundaries and international traveling and trade help disseminate resistant bacteria across the world. This contributes to the complexity of the antibiotic resistance problem and underpins the fact that it is a global issue. Here follows an overview with descriptions of some of the ways resistant bacteria can spread.
Within health-care facilities
Health care facilities are hot spots for resistant bacteria, since many sick people are in close vicinity of each other and antibiotic usage is high resulting in selection and spread of resistant strains. Poor hygiene practices may facilitate spread of resistant bacteria via the hands or clothes of doctors, nurses and other health care staff as well as via patients or visitors. Other risk factors include crowded wards, few isolation rooms, improper cleaning of the facilities and instruments that are used in patient care.
Between people in the community
Bacteria can spread from one person to another through direct contact between people. Transmission can also occur indirectly, for example when someone coughs. If a person contaminates a surface (such as a doorknob) with bacteria, these bacteria can be transferred to another person who touches the same surface. Good hand hygiene is important to limit spread of pathogens and the risk of becoming a carrier of resistant bacteria. Still, even with good hygiene practices, bacteria are a normal part of our surroundings that we will be continuously exposed to.
International travel
International travellers help spread resistant bacteria across the world. Any given day several million people will catch a flight, and if someone carries a resistant bacterium they will bring it along. Many studies have demonstrated that a large proportion of international travellers acquire resistant bacteria during visits in areas with a high prevalence of resistant bacteria. In some studies, more than 70% of people travelling to certain geographical areas were colonized with multidrug-resistant ESBL-producing bacteria upon return. The risk is even higher for hospitalized patients, who are exposed to additional risk factors such as surgery and antibiotic therapy. Several hospital outbreaks have originated from patients transferred from another hospital with a higher prevalence of resistant bacteria.
From animals to humans and from humans to animals
Bacteria can spread from animals to humans, but also the other way around. Many people come in close contact with animals in their daily life as we keep them as pets in our homes or raise animals for food. Resistant bacteria are common in livestock and there are several examples of how farmers and their families have become colonized with the same resistant bacteria as their animals. Likewise, livestock veterinarians are at risk of carrying livestock-associated resistant bacteria. The bacteria may then spread further in society. Resistant bacteria are also found in wildlife and migratory birds but this probably has a limited impact on the increasing rates of resistance in humans.
Food
In many animal farms, antibiotics are used in large quantities to prevent and treat infections as well as for growth promotion, and therefore many farm animals have become colonized with antibiotic-resistant bacteria. During slaughter or when processing the meat, these bacteria can potentially be transferred to the product. Furthermore, fruits and vegetables can become contaminated with animal feces directly from the animals or via contaminated water that is used for irrigation of the crops. Eating food contaminated with bacteria may directly cause an infection, such as diarrhea caused by Salmonella, Campylobacter and E. coli. Resistant bacterial strains, or genes encoding resistance, may also be transferred to the normal flora of the consumer without causing an infection. The resistant bacteria can potentially cause infections later on and spread to other people.
Resistant bacteria are frequently detected in chicken and meat. However, the impact this has on human health is currently not known and may differ in different parts of the world. Some studies demonstrate similarities between the antibiotic-resistance genes found in meat and those found in human pathogens, while other studies have not seen this connection. More research is needed to determine the scale of the problem. Proper cooking and handling of food helps to decrease spread of infections as well as resistant bacteria.
Water
Bacteria can spread via drinking water or water supplies that are used for irrigation, washing cooking utensils or for hygienic purposes. There are many ways resistant bacteria can end up in the water; release of untreated waste from animals and humans is one important source. Resistant bacteria have been found in many water sources such as drinking wells, rivers and effluents from wastewater treatment plants. Several bacterial diseases can spread via contaminated water, including typhoid fever and cholera.
Find out more
Below, you can find links to access factsheets about the spread of antibiotic resistance by ECDC, CDC and WHO. There is also a downloadable PDF containing the slides from the above lecture with Maria Pränting.
© Uppsala University
More from "Part 2"
- Bacteria basics
- Bacterial evolution and importance of normal flora
- Antibiotic basics
- A doctor’s reality
- An ethical dilemma
- Antibiotic use in humans
- Antibiotic use in animals
- Introduction to antibiotic resistance
- Emergence and spread of antibiotic resistance
- Infection prevention and control in the clinic
- Antibiotics and resistance (quiz)
- Test your understanding II
- Reflection and analysis: optimizing antibiotic use on poultry farms
- End of part 2
